To Shield or Not To Shield…THAT is the Question.
Update: Listen to the One Hour Podcast with a Co-Author from the AAPM article – Dr. Marsh
Update #2: Excellent news! The ACR has released a statement that they “will be reviewing the Practice Parameters and Technical Standards in order to make recommendations for alignment with this position statement..” (source)
There is a big buzz going around the imaging community right now and it’s causing quite a stir. The topic centers around the recent announcements that we should stop offering lead shielding to our imaging patients.
Wait, what?!
Radiologic Technologists are taught to shield patients when appropriate in accredited radiography programs. It is ingrained in our psyche from day one of Xray school.
Thyroid shields, gonad shields, and aprons of all sizes.
A recent Facebook post in a radiology group incited some incendiary discussion that proves the staunch support of radiologic technologists to continue to protect their patients from excessive radiation to the best of their ability.
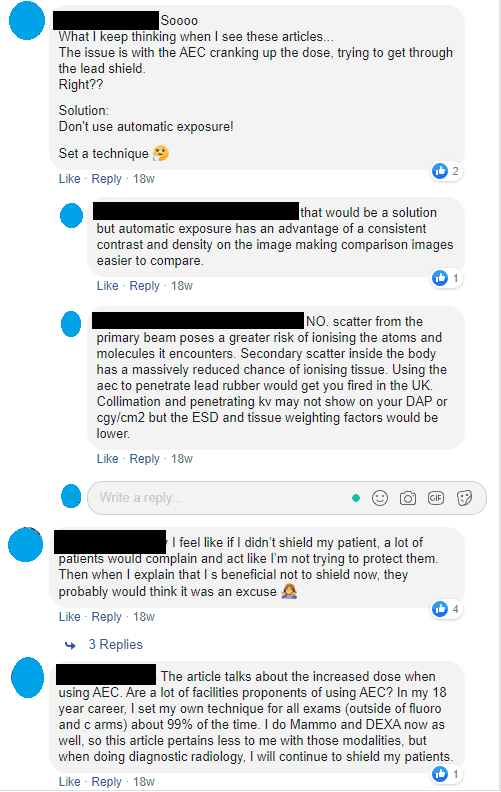
It is going to take a lot more than an “announcement” to convince radiologic technologists to stop using lead shielding on their patients.
Enter Stage Left – The AAPM
But the American Association of Physicists in Medicine (AAPM) is arguing against shielding.
They are reporting that shielding can “obscure anatomic information and interfere with the automatic exposure control of the imaging system.”
The actual AAPM policy that discusses the cessation of shielding is titled Policy #PP 32A, AAPM Position Statement on the Use of Patient Gonadal and Fetal Shielding. (source)
Their basic argument is that shielding can both potentially compromise the exam (leading to repeats) and can negatively affect the automatic exposure control (AEC.)
The latter is, in my opinion, the single biggest question on the minds of many technologists because of the statements in certain circles that shielding increases the dose to patients.
Examine the AAPM References
Among the ten references the AAPM cites, two are the American College of Radiology.
Both of the ACR citations revolve around Practice Parameter Resolutions #39 and #40.
But the second paragraph of the Preamble in Resolution #39 and #40 states “Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care.”
Clearly, the language here is meant to dissuade the use of these Resolutions in a court of law but doesn’t that bring pause to the idea of using them as standards in general?
Call me crazy but if you are making an argument to persuade me to alter my patient care while telling me that it might not hold up in a court of law to protect me from being sued for said care…I’m not too comfortable moving forward.
Perhaps the ASRT is going to step up and offer protection via their own resolution?
How Shielding Increases Radiation Dose
So, let’s look at some of the other eight citations that the AAPM used to fortify their stance to cease all patient shielding during radiographic examinations.
The first is a reference to an article in the American Journal of Radiology. The authors of this article agree with the premise put forth by the AAPM but also add that shielding “carries a substantial risk of increasing patient dose.” (source)
The takeaway is that each imaging technique depends on the system optimizing image quality by adjusting the radiation output based on what is in the imaging Field of View (FOV.)
Although using shielding can greatly improve the consistency of image quality (signal intensity, noise properties, and other factors), the consequence of introducing a highly attenuating material (lead) into the imaging area is significant.
If a lead shield, which is meant to protect the patient, enters the imaging FOV, the radiographic system will “drastically” increase the tube output to try to penetrate the shield.
This results in an increased dose to the patient and a marked degradation in image quality. (source)
Using lead in the FOV increasing dose to the surrounding area.
The Onus is on the Technologist
The AJR readily admits that shielding patients have been a long-standing practice in the field of radiography and that ceasing the practice may cause concern to the patient.
Their remedy for this concern is for the technologist to properly inform the patient upon greeting them for their exam.
Wait, what?!
The AJR article continues: “It may be appropriate to inform the patient that the facility does not provide patient shielding for imaging examinations because evidence indicates that shielding increases the risk to the patient and provides negligible or no benefit.” (source)
Oh, that’ll go over well…
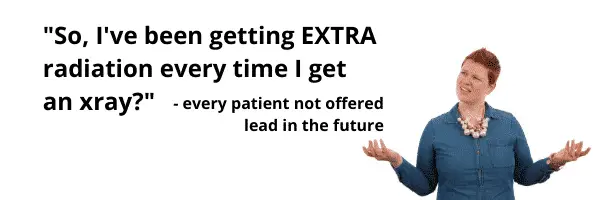
When this policy rolls out at your facility, anticipate questions from patients like this:
- What do you mean it increases my risk? My risk of what? Cancer?
- How do I know if I have received too much already?
- How come you’ve been shielding me my whole life?
- Can I get tested somehow to see how much radiation I’ve received?
- and on and on…productivity will drop and tech blood pressure will rise
But sometimes it is okay to shield…if it makes the patient happy.
The AAPM concedes that if shielding a patient due to their own fear and anxiety will allow the capture of a better quality image, go ahead and shield the patient.
So, given that we now KNOW that shielding may cause an increase in patient dose…it’s okay to use it if the patient asks for it?
Should we get that in writing on a consent form?
The Advancement of our Equipment
Technology has advanced tremendously over the past decade.
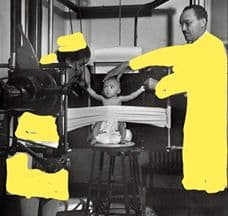
It has been 40 years since patient shielding was first introduced into the US Code of Federal Regulations in 1976. (source)
In those days, an AP pelvis of a 4-year-old male’s testes was registering at approximately 2.5 mGy. By 2012, that dose has been reduced to 0.06 mGy or the reduction of more than 96% thanks to advances in technology.
There’s no denying that.
In addition, the original intent of the Federal Regulation was to protect against genetic mutation NOT stochastic effect against the patient.
So it was to protect the offspring of the patient getting radiation, not the patient themselves.
Here we are, 42 years later and there are still no hereditary effects from radiation that have ever been observed in humans. (source)
Time to Get Educated on this Topic.
Then there’s the ICRP Publication #103. For those unfamiliar, the ICRP is the International Commission on Radiological Protection.
You can read more about them here but know that it has been around since 1928.
The ICRP had input from the following organizations:
- The International Radiation Protection Association
- The Nuclear Energy Agency of the OECD
- The European Commission
- The United Nations agencies, with the International Atomic Energy Agency as the lead agency
- and, of course, the ICRP
So this isn’t just one or two groups chiming in here. This group consists of hundreds of experts.
Publication #103, page 91, section 224 states “Societal values usually influence the final decision on the level of radiological protection.
Therefore, while this report should be seen as providing decision-aiding recommendations mainly based on scientific considerations on radiological protection, the Commission’s advice will be expected to serve as an input to a final (usually wider) decision-making process, which may include other societal concerns and ethical aspects, as well as considerations of transparency (ICRP, 2006a).
This decision-making process may often include the participation of relevant stakeholders rather than radiological protection specialists alone.” (source)
In other words, it isn’t so cut and dried after all. There are a lot of different factors weighing in here beyond the science of dose. Namely cultural history, patient education, and staff protection.
The science is there, change is coming in our practice.
The voices of reason are starting to talk louder. It is incumbent on all technologists to become familiar with this topic and understand the merits of the science.
This initiative is coming and that right soon.
I, for one, will feel a lot better if someone offers a policy that we can lean on for protection as technologists.
Especially since we’re the ones on the front lines who are going to get the blowback from the patients.
Technologists – please educate yourself. You have the training and the wisdom to educate patients.
“If the sources of reason and wisdom in the community are silent, only irrational and foolish voices will be heard.” (source)
Listen to the One Hour Podcast with a Co-Author from the AAPM article – Dr. Marsh
Let our community know what you think about this topic by posting a comment below.