How to Cope and Deal with Osteoarthritis
Osteoarthritis is not just one single disease as we may have understood decades ago.
It is an illness that can be related to joint pain and degenerative joint disease.
Though this is a widespread concern, we failed to understand it completely.
This disease which attacks us in many different types, do not bias and targets all age groups, genders, and communities.
However, women and older adults are more prone to this disease.
Common Symptoms
A common symptom of this disease is the swelling and stiffness in the knee, which is painful.
The pain can limit us from doing our normal physical activities.
Symptoms can be erratic and may result in mild or severe pain.
Arthritic knee pain causes difficulty while bending and stretching the knee.
Osteoarthritis is one of the most significant causes of disability in adults in the United States.
Types of Arthritis, like Osteoarthritis:
Let us discuss some of the types of arthritis briefly.
(1) Osteoarthritis (OA):
It is the most common type of arthritis that eats away the joint cartilage; a firm and flexible connective tissue, in a slow process.
You will experience discomfort in your physical movement, like climbing upstairs, which will also be visibly red around the knee.
The pain is also likely to occur in other parts of the joint such as synovium (fluid), bone and ligaments.
This illness is most likely to occur after middle age.
2. Rheumatoid Arthritis (RA):
This affects the joints and other body organs; the attack comes from the body’s immune system.
The bacteria in RA becomes excited and destroys healthy tissues in the body.
Moreover, You may quickly get tired, experience a loss of appetite, and fever and red-blood-cell count may also decrease.
In other words, you may be anemic. The immune system attacks the synovium and leaves permanent damage causing deformity if overlooked.
The pain can also occur in the bones and ligaments. Most people suffering from this disease have antibodies known as rheumatoid factors (RF) in their blood.
There is a common blood test you can take to test for this.
3. Psoriatic Arthritis:
This auto-immune inflammatory arthritis affects people who have psoriasis.
Psoriasis is a skin disorder causing redness, scaly rash on your elbows, ankles, knees, feet and other parts of the body.
The disease can either be mild or severe, and the symptoms are usually swollen joints, stiffness, and pain.
Damage can worsen if left untreated.
4. Thumb Arthritis:
This disability occurs when the cartilage wears away at the base of the thumb joints.
It causes severe pain and swelling, making it challenging to turn doorknobs, opening jars, etc.
So, This type of problem requires splints and medication and surgery for severe arthritis.
5. Septic Arthritis:
This includes a painful infection in a joint caused by germs traveling from other parts of the body through the bloodstream.
It can affect the hips, shoulders and other joints besides the knee. Children and older adults are more vulnerable to it.
Antibiotics and needle draining of the connective bones are usually a remedy for Septic arthritis.
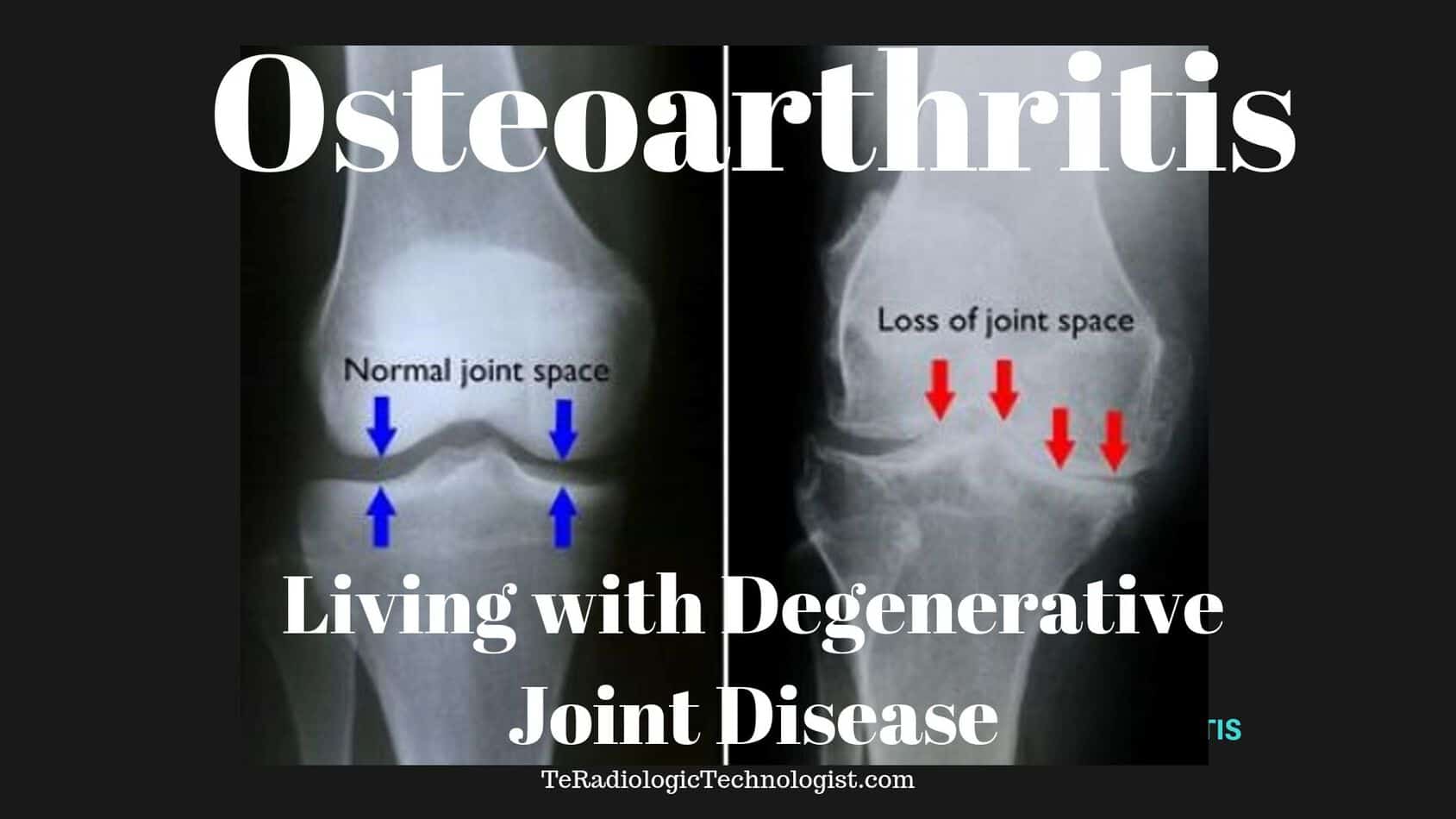
How Accurate is a Knee X-Ray for Osteoarthritis?
X rays can help a doctor see the inside of the joints painlessly. They are typically the gold standard for examing the knee for osteoarthritis.
For further evaluation after the xray, patients can get a CT scan or an MRI exam.
These are the several types of imaging exams that can scan for arthritis:
(1) X-ray (Radiography):
It is a simple test where an X-ray beam passes through the knee, creating a double-dimensional image of the bones forming the joints.
This process gives details of specific dense structures like bone, bone spurs, and large effusions.
They are highlighted and appear white on film. However, diagnosing soft tissue like muscle, tendons, ligaments and the meniscus are vague and appear grey, providing very little detail.
An X-ray can be called for if the patient has been experiencing knee pain for several weeks.
Moreover, These types of Xrays should take about ten minutes. These are what I trained to do for the last twenty years.
2. Computerized Axial Tomography (CAT or CT):
This scan produces multiple images of the knee, combining every single image and creating a three-dimensional picture.
The scan detects soft tissues better than other conventional Xrays.
Moreover, This exam can take from 10-15 minutes.
3. Magnetic Resonance Imaging (MRI):
The process involves a strong magnetic field that sends signals to the computer to provide a clear image of both the soft tissues and bones.
The scanning machine produces black and white images and shades of grey of the knee joints.
With the clear details of the tissues visible, this procedure is especially useful to identify injuries to the tendons, ligaments, cartilage, menisci and the swelling area.
Although better detail, this exam can take up to 45 minutes.
The longer the exam, the better the detail…typically.
Diagnosis of Osteoarthritis:
On your visit to the doctor, he will examine you and ask about your symptoms related to arthritic knee pain like swollen joints and a decrease in physical motion.
You will also require a blood test (RF mentioned earlier) and an x-ray, which can help distinguish the type of arthritis you may have.
Let us quickly look into how many ways we can diagnose osteoarthritis.
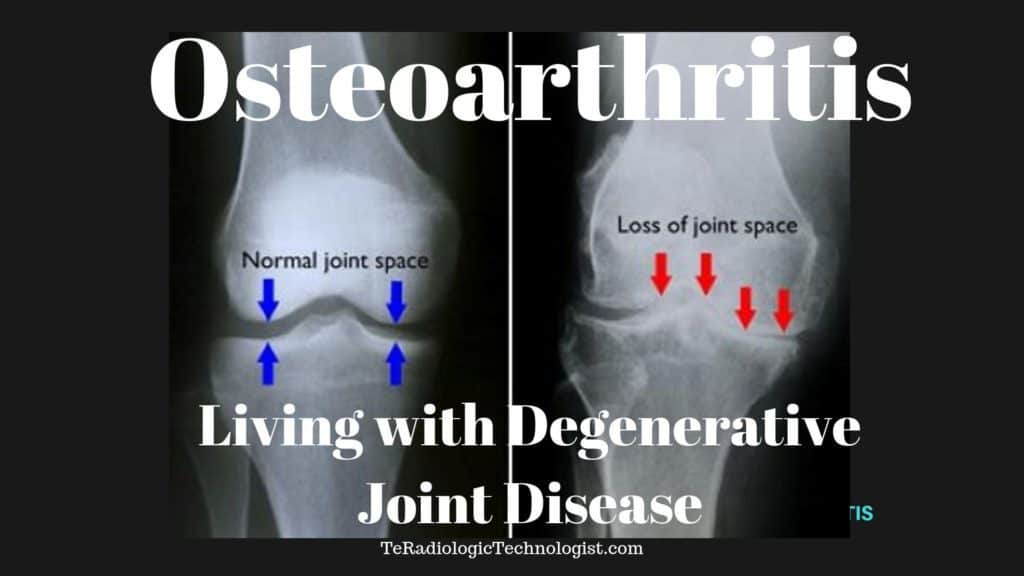
Knee (AP Weight-Bearing View):
Researchers and physicians agree that a standing knee x-ray is essential for arthritis patients rather than the non-weight bearing position.
It is a standard projection to study the knee joint, proximal tibia, fibula, distal femur and the patella (knee cap.)
This standing position is used to get images of the knee with its natural anatomical position and under the stress of normal weight.
Steps:
- The suspected arthritis patient is asked to stand against the upright detector with the back of the knee touching the detector.
- The leg should stretch.
- The knee should not rotate, feet together, toes facing forward.
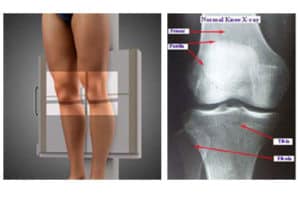
Knee (Rosenberg View)
This is a specialized procedure usually to detect early signs of Osteoarthritis (OA) in suspected patients.
It is the initial study for anyone having symptoms of the disease.
It is more sensitive than the regular weight-bearing view to detect knee joint space narrowing.
Steps:
- The patient will be asked to stand against the upright detector or xray cassette holder.
- With the knees bent forward and touching the detector at about a 45-degree angle.
- This position provides discomfort to the patient but provides better results for the doctor studying the problem.
Tunnel View Knee X-Ray (Knee PA Avial Camp)
Steps:
- The patient is asked to lie in a supine position: lying with face upwards.
- The knee bends from 40-45 degrees with knee support for rest under it.
- It demonstrates the posterior aspect of the femoral condyles, the intercondylar eminence of the tibia, and intercondylar notch.
What Type of Treatments are Required to Treat Osteoarthritis?
There can be several ways to manage the inflammatory pain in the joints; however, there is no permanent cure for it.
Moreover, Check out some of the answers to help you get some relief from this health predator.
1. Exercise:
It is strongly recommended to visit the doctor for advice before you start any exercise regime.
The absence of physical activity can lead to muscle loss, and additional weight gain as this disease can severely reduce the joint motions.
Even with medication, osteoarthritis can significantly affect daily life.
Physical training is recommended for a gradual decrease in pain and stiffness and avoid further damage.
With exercise as a treatment plan, it will help you:
- Maintain normal joint movement
- Increase muscle strength and flexibility
- Keep Cartilage tissue and bone strong and healthy
- Reduce the weight pressure of the joints
- Improve cardiovascular fitness.
2. Arthritis Knee Brace:
Braces are suitable for people with arthritic knee pain. This equipment can help your knee stability while walking and enhance your mobility as it takes off the pressure on the joints.
You can stand and move around with more confidence while this brace unloads the stress generating from the knee joints caused by osteoarthritis.
People using knee braces report that a lot of comfort and relief is provided and relieves the strain they suffer from this disease.
3. Knee Replacement Surgery:
It is also known as knee arthroplasty, which involves a medical process to remove the knee joint weight-bearing base.
This is done mainly to relieve a patient from pain and physical deformity. The surgery is considered to be one of the most common bone surgeries. The decision must be made between you and your doctors.
Knee replacement operation is an option when most of the other treatments you have tried doesn’t seem to give a positive result.
It involves cutting away the arthritic bone and replace it with a prosthetic joint.
There are different types of knee surgery:
Knee replacement:
It is a conventional surgery where the base of the thigh and shin bone connecting to the knee is replaced.
Kneecap replacement:
This procedure involves the replacement of the under-surface of the kneecap
Partial knee replacement:
This surgery is done through a smaller cutting, unlike the total knee replacement. People with arthritis affecting only one side of the knee usually opt for this process.
Complex knee replacement:
A patient who has undergone several knee replacement surgeries or having severe arthritis may be advised to undergo this operation.
Osteoarthritis Do’s:
- Choose activities that build the muscles around the joints
- Add low-aerobic routines like cycling and walking etc.
- Pain relief medication and cream can also be applied for temporary comfort.
- Therapy, acupuncture, and massage, etc. can also be an ideal physical and emotional integration.
- Understanding the condition of the type of arthritis you have and if any of the joints are damaged.
- Involve your doctor, family, and friends to manage the pain.
- Inform your doctor of any changes in the pain.
- Use good posture, regular body motions, balance activities (don’t overdo).
- Manage weight, quit smoking as it stresses the connective tissues.
Osteoarthritis Dont’s:
- Inflammatory foods like fried and processed, sugars, dairy products, alcohol, tobacco, salt, and preservatives.
- Activities involving high impact like running and jumping etc.
- Overconsume pain relief medication.
Alternative Therapy
I’m nearing 50 years old and one thing that is becoming painfully clear to me is arthritis in my hands.
There are days when they feel very tight and just straightening all my fingers out turns them white from lack of capillary blood flow.
One treatment I am experimenting with is Curcumin.
There have been numerous studies that show the efficacy of Curcumin on arthritis, namely:
- chronic inflammation reduction
- reduced occurrences of chronic back pain
- natural blood thinner
I am following the recommended dose listed here to see what the outcomes show.
Since there are no studies that I can find linking Curcumin to negative side effects, this is a win-win for me if I get just one of the positive side effects listed above.
Moreover, I believe that I will see a reduction in my hand swelling and possibly even see some reduction in my blood pressure medication use.
Conclusion:
As a radiographer, I ‘ve seen thousands of patients with joint diseases over my career.
It causes pain and makes life more difficult to enjoy. You won’t know when it will occur but you can try to integrate some of the joint-saving techniques mentioned.
I have tried to do zero-impact exercises for the last 30 years in an effort to stave off arthritis.
Exercises like swimming and bicycling put zero to minimal weight on the joints.
My mom used to run marathons when I was a child. Now in her 70s, she has ruined her knees and hips with all that concrete pounding while running.
People having arthritis should try to maintain a healthy lifestyle, visit the doctor regularly, and continue taking the prescribed medications.
Easier said than done, right?
This worldwide disability can severely affect our daily activities and limit our movements if left untreated or attended.
Take precautions against the disease early and consult your physician.
Follow the list of examinations prescribed by your physician and get the Xrays, CT scans or MRI exams, and blood tests.
The doctor will need these to properly diagnose your pain.
Reference:
Glyn-Jones, S., Palmer, A. J. R., Agricola, R., Price, A. J., Vincent, T. L., Weinans, H., & Carr, A. J. (2015). Osteoarthritis. The Lancet, 386(9991), 376-387.
Loeser, R. F., Collins, J. A., & Diekman, B. O. (2016). Ageing and the pathogenesis of osteoarthritis. Nature Reviews Rheumatology, 12(7), 412.